COVID-19 Practical Tools for Your Practice

As of March 30, 2020, 27 states have taken steps to help lessen the spread, e.g. stay-in-place-order requesting individuals to remain at home except for the most essential reasons, such as grocery and pharmacy shopping or essential business-related reasons. This encompasses approximately two-thirds of the country’s population. Additionally, numerous states have also implemented executive orders limiting the scope of medical practices to only “medically critical or necessary” procedures and or surgeries. As such, many practices are scrambling as nonessential surgeries have been canceled, placing many of our member practices at near term risk.
Recognizing that we have multitudes of resources available to us at our fingertips, the AVLS Board of Directors has developed a more concise library of key resources designed to help guide members through the COVID-19 pandemic as we seek to protect our patients and our practice teams from the impact this is having on all of our lives.
“We all recognize the impact that this pandemic is having on our membership, our patients, and our livelihood. There will be a downtime and we are all suffering, but we’ll get through this and be stronger than ever.” Marlin Schul, MD, MBA, RVT, FAVLS, President AVLS.
Re-opening
The following resources are available to guide your decisions around safely re-opening your practice.
From the Front Lines
Linda Antonucci, RPhS, RVT, RDCS has been volunteering with a COVID-19 testing site. She has shared her experiences with us:
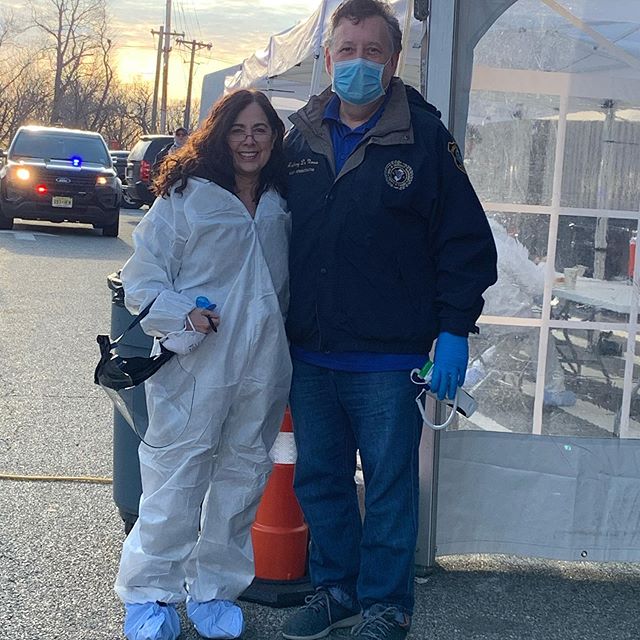
"I believe that one should be generous with his or her time and talents, so it was natural for me once my clients canceled their hours that I would use medical skills as a volunteer. The perfect opportunity opened-up when my county (Passaic County, NJ) began a free COVID-19 test site and were seeking volunteers. What made this opportunity more attractive is that my brother is the county administrator, and I would also serve my community, my current residence as well as the city where I spent my early formative years.
It’s drive-thru test site, where the cars are greeted and patients registered before driving to an area where the they are swabbed to test for the virus. I arrive at the site at 7:15am, get my temperature checked, then I don my hazmat suit, N95 mask, face shield, booties, and three pairs of surgical gloves. I am well protected. I’ve done almost every job so far – I began greeting patients, logging in their information in a laptop, and then moved up to collecting specimens. Swabbing will be my next and final job.
There is a positive camaraderie between all the volunteers, which is good because it off-sets some the obvious sadness of this affair. There is a palpable fear among the patients getting tested. You can see in in their eyes as they peer above their masks. One patient was so ill she expired in the backseat of her car while she was waiting to get tested. The only thing I know about the patient is that she was Hispanic and waited until the free test opened because she didn’t have insurance. This incident really brought home the tremendous toll the virus is having on poor under-served communities."
Dr. Kathleen Gibson, AVLS Board of Directors' Secretary, has been working at ground zero for COVID-19 in the US. This video offers insight into how Kathy's team has responded and the personal toll COVID-19 is taking on healthcare workers.
Updates from the AVLS
Practice Guidelines
With numerous states issuing orders to restrict the scope of practice during the crisis and others wondering what the correct and proper decision is to make, the Society recognizes that many are faced with difficult decisions that will impact the livelihood of our patients, our staff and our very businesses. And as such, we recognize that we are not in a position to make such recommendations one way or the other as this is an individual decision.
That said, we would like to provide some resources to help you navigate the decision process for the immediate and short-term while also consideration for how to approach the future when we begin to restart our practices in the coming weeks. AVLS members should follow the guidance set for by the CDC and their individual state governments.
Staffing Challenges and Best Practices
By Dr. Ron Winokur and Linda Antonucci
Although vein disease is important to patient’s quality of life, practitioners in hospital-based practices and private offices can help maintain a healthy workforce and availability of resources to decrease the burden on healthcare systems. The goal of this section is to provide guidance on methods to maintain appropriate staffing during this unprecedented time while still providing availability for urgent patient needs and minimizing the risk of the spread of Coronavirus. Private offices and hospital-based practices have different challenges that will be barriers to the implementation of these practices.
Best practices:
- Monitor staff for fever or flu-like symptoms
- Prevent staff from working if they have developed symptoms
-
Divide office staff into teams that alternate weeks in-office
- Out-of-office staffing team handling telemedicine, patient screening, and administrative tasks
- In-office staffing team focusing on in-person medical care to those patients that truly need it
- Rotating teams utilizes less personal protective equipment, exposes fewer staff members, and creates the environment to offer care to those with the greatest need for superficial or deep vein care.
- Limit patient scheduling to prevent overcrowding in waiting room or need for excessive staff
- Limit procedure scheduling to required procedures
- Keep your staff and patients safe
Additional Resources:
Personal Protection Gear & Current Guidance for COVID-19
By Dr. Yung-Wei Chi and Dr. John Blebea
Regardless of your specific situation regarding scope of practice restrictions we are all faced with the concern of how to protect our patients, our staff as well as ourselves.
Recommendations are tempered by available local resources. However, in most situations, it is both advisable and practical to:
- Wear a face mask throughout the day while in the office, both yourself and all nursing and administrative staff. Although homemade masks provide some protection, a standard surgical mask is much better. Due to shortages, an N95 respirator is recommended only when in the presence of infected individuals. It does, however, provide much better protection against viruses than surgical masks. A single mask can be worn throughout the day.
- Wear gloves and wash, while wearing the gloves, with soap and water for 20 seconds before and after examining each patient. Current recommendations are to use soap and water rather than alcohol-containing disinfectants because of concern that the latter may impair glove integrity.
- A separate face shield is not recommended unless aerosol-inducing naso-pharyngeal procedures are being performed.
- To the extent possible, maintain physical distancing of six feet between office staff.
- When arriving at the office, change into surgical scrubs or other garments which are removed at the end of the day and are laundered, but not taken home.
- Although not specified by any guidelines, many health care workers in regions with high numbers of COVID infected individuals leave their shoes in the garage before entering the house. If they have not worn separate garments in the office, they take off their work clothes, put them in a separate plastic bag to be laundered, and take a shower before changing clothes and coming into contact with their family members.
Additional Resources:
Embracing Telemedicine
By Dr. Chris Pittman and Dr. Margaret Mann
As you are facing the impact of COVID-19, we urge you to consider implementing telemedicine in your practice. This is about social distancing, lessening the spread, and keeping you, your staff, and your patients safe during this pandemic while also preparing for the time when our practices begin to reengage in normal operations.
Telemedicine has been around for many years, but difficult to monetize. New legislation has opened up reimbursement paths and each payer has identified value in using technology.
Seeing patient’s faces, communicating eye to eye with them about their situation and how we can help is more than amazing. Telemedicine allows us to keep the pipeline growing and keep patients engaged until we can safely bring them into the office for ultrasound studies and treatment.
How to get started
First, there are many HIPAA compliant telemedicine platforms currently available. Check with your EMR/Practice Management system, a majority already have integrated with third-party vendors.
Other platforms are also readily available such as Skype for Business, Updox, VSee, Zoom for Healthcare, Doxy.me and Google G Suite Hangouts. These have stated that their products will help physicians comply with HIPAA and that they will enter into a HIPAA BAA (Business Associate Agreement). Implementing a solution that has or will be able to provide HIPPA compliance, in the long run, is recommended as we believe that telemedicine will become an ongoing part of all our futures following this crisis.
However, in the current crisis environment, HHS has relaxed the rules pertaining to HIPAA compliance allowing for multiple modes of communication including Apple FaceTime, Skype, Google Hangouts, and telephone communications.
Telemedicine Billing Guidance
At this time many payers are waiving patient co-pays for telemedicine visits. Be sure to confirm this with the payer in advance.
Although payer approaches may differ, one of the tenets is to use standard E&M codes 99211-99213 and 99201-99203. The place of service should be reported as ‘02’. Modifier 95 or GT should be reported for telemedicine visits.
It is important to review the modifiers to report accurately what was done with the patient.
For example, ulcer patients can show you and measure their ulcer dimensions. Or patients with swelling can take measurements of their limbs with little difficulty. Document the time spent accurately. We encourage you to record video/audio of the visit if possible. When recording a patient visit, you must request consent to record at the beginning of the visit. It is important that you handle a telemedicine interaction with the patient just as you would an in-person consultation and that you go through the same process as if the patient entered the practice to support your documentation.
Additional resources are becoming available each day from a variety of payers. The following is some recently posted payer guidance for telehealth payment.
Payer Guidance:
For Medicare patients, both established and New patient E&M codes can be billed using digital means, web portals, Skype, or Facetime. CMS will now reimburse telehealth visits at the same rate as regular, face-to-face E&M visits. CMS waivers and additional information may be viewed here:
Additional Resources
Financial Relief Opportunities
If you are actively struggling, you may be eligible for a low-interest Small Business Administration loan.
CARES Act
As part of the COVID-19 CARES Act, AVLS members might see today or shortly a direct Federal payment in your practice's bank account as a part of the CARES Act. Providers will be distributed a portion of the initial $30 billion Federal pool based on their share of total Medicare Fee for Service (Part B) reimbursements in 2019. Total FFS payments were approximately $484 billion in 2019.
The distribution policy adopted by the US Department of Health and Human Services (HHS) reflects the recommendations from organized medicine, including the AVLS, made to Secretary Azar earlier this week, with some differences. In part, the difference stems from the administration's approach of first disbursing $30 billion and later determining how the remainder of the funds will be allocated.
MANY AVLS MEMBERS WILL RECEIVE A PAYMENT - THIS MONEY DOES NOT NEED TO BE PAID BACK.
A provider (NPI or TIN for groups) can estimate their payment by dividing their 2019 Medicare FFS (not including Medicare Advantage) payments they received by $484,000,000,000, and multiply that ratio by $30,000,000,000. Providers can obtain their 2019 Medicare FFS billings from their organization's revenue management system. As a rough estimate, a physician or practice would receive $61,983 for every $1 million in Medicare FFS billings. Likewise, a practice with $500,000 in FFS billings would receive $30,991.
Specific details, terms, and attestation instructions are on the HHS website:
CMS Relief Program
The AVLS naturally encourages members to understand in detail your own financial metrics, but we suggest members approach with caution the new CMS Advance Payment Program. The CMS Advance Payment Program is not a grant or forgivable loan program. CMS will start to recoup the money advanced to your practice after 120 days. Many vein clinics operate on a delay in cash flow of approximately 60-120 days, so once patients start to come back for care after COVID-19 abates, you may be faced with "negative" Medicare payments for several months.
AVLS Webinars
| Past | Best Practices for Employers Regarding COVID-19 by Fischer & Phillips LLP | View Recording |
| Past | Do's and Don'ts of Telemedicine by Shumaker, Attorneys at Law | View Recording |
| Past | Navigating the COVID-19 Pandemic and the Government's Response - An AVLS Legal Townhall by FisherBroyles, LLP | View Recording |
| Past | Navigating the Financial Turmoil of COVID-19 by Shumaker, Attorneys at Law | View Recording |
| Past | The Physician Employee by Shumaker, Attorneys at Law | View Recording |
| Past | The Future is Here, Introducing the Hybrid Practice by ClinicGrower | View Recording |
| Past | Coming Out of the COVID-19 Crisis: Modifying Your Digital Marketing Strategy by MD Connect | View Recording |
| Past | Marketing Strategies To Implement Now For Your Vein Practice by Healthcare Success | View Recording |
| Past | The Five Pillars of a Successful Virtual Practice by Doctor.com | View Recording |
| Past | Beyond Groundhog Day: Moving Forward with your Practice | View Recording |
AVLS Webinars are made possible thanks to a grant from the Foundation for Venous & Lymphatic Disease.
Additional Educational Resources
Please note that we acknowledge this is not a complete listing of all available resources available to you during this crisis but is simply a tool to help guide you in the direction of recourses to enable you to make the most informed decisions.